Pulmonary Hypertension
The Wesley Pulmonary Hypertension Unit
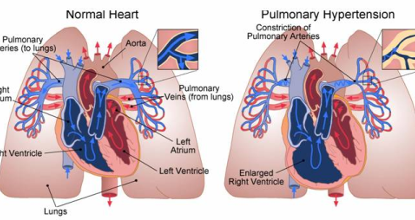
It is an uncommon form of high blood pressure that can adversely affect the arteries and blood vessels in the lungs and cause damage to the right side of your heart.
Pulmonary arterial hypertension is a chronic, life limiting disease that is caused by an increase in blood pressure within the pulmonary vasculature due to the blood vessels being narrowed, blocked or destroyed over time. This progressive damage means the pressure in the pulmonary arteries rise and the heart has to work harder to pump blood through to the lungs. This extra effort can eventually lead to right heart failure as the muscles become weaker over time.
The symptoms of pulmonary hypertension are particularly non-specific making it difficult to initially distinguish from many other diseases and conditions and as such, the formal diagnosis of pulmonary arterial hypertension can be significantly delayed. As this disease progresses, its symptoms can be noted more frequently and with less exertion.
Symptoms Can Include:
- Shortness of breath ( dyspnoea) particularly when walking up hills or climbing stairs but this shortness of breath can also be noted when at rest
- Fatigue
- Chest pain
- Dizziness or fainting (syncope)
- Swelling (oedema) in your legs, ankles and even you abdomen
- Bluish colour to your lips/skin (cyanosis)
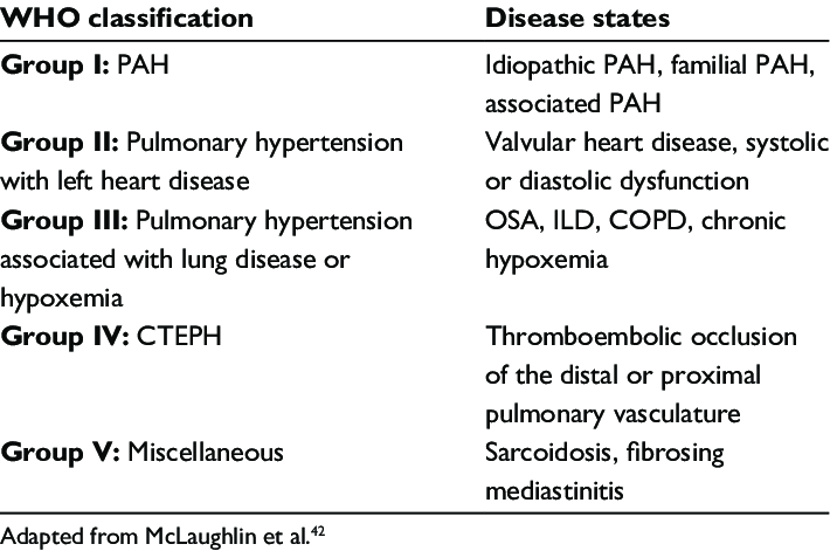
Pulmonary hypertension is classified into 5 groups depending on its cause. These groups dictate appropriate and available treatment options.
Early screening is the key to the timely diagnosis of pulmonary hypertension and it recommended in high risk groups of people including:
- A family history of pulmonary hypertension
- People with connective tissue diseases, particularly those diagnosed with scleroderma/SLE
- People who have had a previous pulmonary emboli (blood clot/s in the lungs)
- People with congenital heart disease
Most of our patients are referred to the clinic with unexplained breathlessness, decreased exercise tolerance and/or abnormalities on an echocardiogram. Further investigations may need to be conducted prior to your appointment in an effort to expedite a diagnosis and can include:
- Breathing test (Complex Lung function Testing)
- 6 Minute Walk Test
- Further medical imagine including a V/Q scan or CTPA (To look for blood clots in the lungs) and a High Resolution Chest CT Scan
- Blood tests
During your consultation, the results of these tests will be discussed and you will also be asked questions about your medical history, previous and current medications including dietary pills, alternate therapies and any history of stimulant usage as all of these have the potential to cause pulmonary hypertension.
If the tests that you have had indicate a high probability for pulmonary hypertension, you will likely be referred to a cardiologist who has an expertise in performing Right Heart Catheters to undergo a Right Heart Catheterisation to confirm this suspected diagnosis.
This is typically a day procedure that allows the doctors to directly measure the pressures in the right side of the heart including the pulmonary artery pressures, cardiac output and pulmonary capillary wedge pressure. A right heart catheter is considered the ‘Gold Standard’ for the diagnosis of pulmonary hypertension and is required by Medicare when applying for any medications that are used to treat this disease.
.
While there is no current cure for pulmonary arterial hypertension, there are several different medical therapies available via the PBS to help manage your pulmonary arterial hypertension. These therapies can include tablets, inhaled and intravenous modes of delivery.
These treatments can be used singularly or in combination depending on the severity of your pulmonary hypertension.
